Protecting customers, the public and employees from legionnaire’s disease is an incredibly important responsibility for any hotel. Over 300 cases of Legionnaire’s disease are reported annually, with the large majority of these diagnoses being easily avoidable.
What is Legionnaire’s Disease?
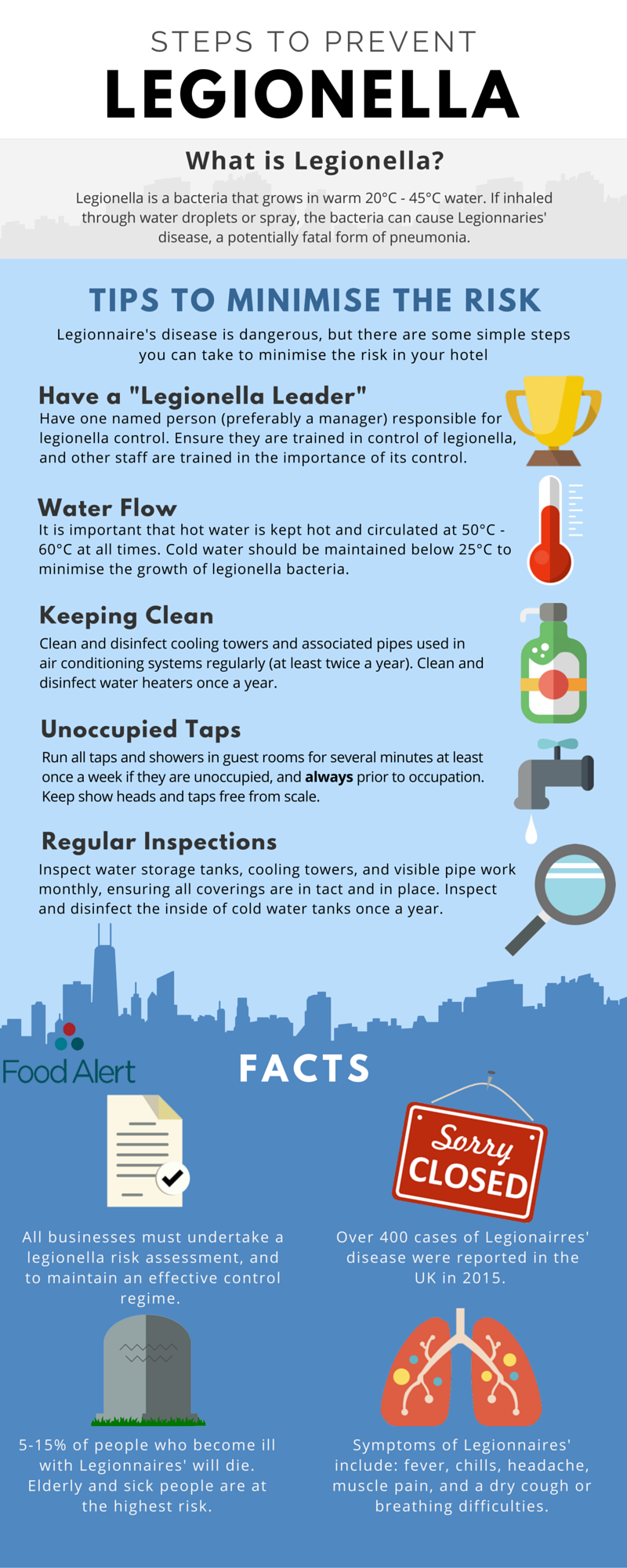
Legionnaire’s is a potentially fatal disease caused by legionella bacteria, which may be present in tepid water. It is spread by the inhalation of the legionella bacteria through water droplets or spray. Elderly people, children, and those weakened by sickness are at the highest risk of contracting the disease, symptoms of which include high temperature, a cough, and chest pains.
The Law
The Control of Substances Hazardous to Health Regulations 2002 (COSHH) requires all businesses to undertake a legionella risk assessment, and to maintain an effective control regime. Failure to comply with the legislation can results in huge fines.
Even if no outbreak has occurred, prosecution can still be considered where a water system which poses a risk has been found; a suitable and sufficient risk assessment has not been carried out; or the necessary precautions/monitoring to control the risks have not been taken in accordance with the Approved Code of Practice.
If you are an employer, or someone in control of premises, including landlords, you must have a person in place that understands the health risks associated with legionella.
The person responsible for managing risks, need to understand your water systems, the equipment associated with the system such as pumps, heat exchangers, showers etc, and its constituent parts. They must be able to identify whether they are likely to create a risk.
High Risk Areas
Legionella bacteria can be present wherever water droplets can be created. This means the main sources of outbreaks are from:
- Showers and taps
- Swimming pools and whirlpool baths (Jacuzzi’s)
- Cooling towers and evaporative condensers used for air conditioning, even if they are situated on the roof or in the grounds
- Ornamental fountains, particularly indoors
- Humidified food displays
The bacteria can multiply anywhere water is at a temperature between 20-45°C. The most common locations for bacterial growth are:
- Large/ stagnant water tanks
- Pipes with little or no water flow (including unoccupied rooms)
- In slime and dirt in pipe and water tank
- Rubber and natural fibres in washers and seals on the water systems
- Water heaters and hot water storage tanks where the temperature of the water is below 45oC
- Scale on shower heads and taps
- Wherever there is a source of nutrients such as rust, sludge, scale, organic matter and biofilms
Reducing the Risk
The risk of Legionnaires disease form domestic water supplies can be minimised by:
- Having a Legionella risk assessment carried out by a Competent Person.
- Appointing a trained member of staff to be responsible for legionella control, other staff should also be trained in the importance of legionella control.
- Keeping the hot water circulating and in storage between 50-60°C, and cold water below 20°C.
- Flushing outlets which are not often used. Running the water for a few minutes should be sufficient.
- Running all taps and showers in guest rooms (where present) at least once a week if they are unoccupied.
- Descaling shower heads and taps every three months.
- Monitoring temperature control monthly, alongside random tap temperatures.
Whirlpool baths are generally kept at around 40°C when in use, making them the perfect temperature for legionella to multiply. The Landmark Hotel in Dundee were faced with a £54,000 when their hot tub infected 65 customers and staff with the disease. To minimise the risk of bacteria spread, special care must be taken:
- It must be continuously treated so 2-3 mg/l chlorine or bromine is present in the whirlpool, and the levels are monitored at least 3 times a day.
- At least half of the water is replaced each day.
- Sand filters are backwashed daily.
- The whole system is cleaned and disinfected once a week.
Your Risk Management Assessment
Your risk management assessment should include:
- management responsibilities, including the name of the competent person and a description of your system
- competence and training of key personnel
- any identified potential risk sources
- any means of preventing the risk or controls in place to control risks
- monitoring, inspection and maintenance procedures
- records of the monitoring results and inspection and checks carried out
- arrangements to review the risk assessment regularly, particularly when there is reason to suspect it is no longer valid
Keeping records:
If you have five or more employees you have to record any significant findings, including those identified as being particularly at risk and the steps taken to prevent or control risks. If you have less than five employees, you do not need to write anything down, although it is useful to keep a written record of what you have done.
Records should include details of the:
- person or persons responsible for conducting the risk assessment, managing, and implementing the written scheme
- significant findings of the risk assessment
- written control scheme and details of its implementation
- details of the state of operation of the system, i.e. in use/not in use
- results of any monitoring inspection, test or check carried out, and the dates
These records should be retained throughout the period for which they remain current and for at least two years after that period. Records kept in accordance with (e) should be retained for at least five years.
Water safety and protection from Legionnaire’s disease is of the highest priorities for hotels and B&B’s. For absolute peace of mind in ensuring water safety, talk to the experts. For more information about how Food Alert can protect your business contact us at enquiries@foodalert.com or call us on 020 7244 1900.